


This page contains relevant information to assist those faced with an emergency situation in the Greater Wangetti Region. The information contained herein was current in December 2024 and the treatment information was sourced primarily from St John Ambulance Australia, Australian Red Cross and Health Direct (Australian Government). See "Dangerous Fauna" and "Dangerous Flora" to identify potential threats to your safety.
DISCLAIMER - The utmost care has gone into the making of this page. We believe the information is true and correct at the time of publishing. We cannot and will not, however, be held liable in any way for any injuries or deaths by any persons who have been treated using the information on this page. If you are unsure, please wait for the paramedics or a doctor.

In the case of a serious emergency it is always prudent to call 000 and request the relevant emergency service. This is of course sound advice, but please bear in mind that mobile phone reception in and around Wangetti is patchy and predominantly only via Telstra. If you are out of range from the Wangetti Telstra tower, but are on higher ground and have line of sight to either Buchan's Point or Island Point, you should have reception on any of the 3 main carriers. There is an Optus tower above Turtle Cove but, due to the adjacent terrain, reception is localised. Usually there is no reception along the Cook Highway, between just south of Quaids Road and the South Wangetti Carpark. As you move westward into the hills, reception is extremely patchy. Wangetti Beach has reasonable reception at the north end, but becomes patchy the further south you go.
Telstra - is the only carrier that functions within the actual township of Wangetti. Heading north, it provides continuous service along the highway, from just south of Quaid's Rd to Oak Beach and beyond. Heading south on the highway, there is a dead area from just south of Quaid's Rd until you reach the Wangetti southern carpark. From there, reception is good through to Palm Cove and beyond. There is good reception from the Wangetti northern carpark, along the beach, until about 60% of the distance to the southern carpark. It then goes dead until about 200 mts north from the southern carpark. The reception is good from that point southwards. As you move west along Quaid's Rd, there is reception for the first 3 kms, then it becomes extremely patchy, until reception is restored as you approach Black Mountain Rd. From there reception is patchy but reasonable.
Optus - has no reception within the Wangetti township. On the highway, reception begins from just north of the Wangetti TelstraTower, and is reasonably good from there north. Heading south on the highway, reception begins again at Red Cliff Point, just south of the Wangetti southern carpark. From there it is reasonably good through to Palm Cove and beyond. There is reception at the Wangetti northern carpark, and this continues for about 60% of the beach, heading south. The remaining beach area and southern carpark has no reception. Heading west on Quaid's Rd, there is no real reception until you reach Black Mountain Rd. From there the reception is patchy.
Vodafone - offers similar reception to Optus, but is more patchy along the highway, both to the north and to the south. It has no real reception at all, as you move westwards.
If your phone is showing "Emergency Calls Only", that means you are within the Telstra network and you can call 000 in an emergency, no matter what carrier you are using.
The absolute best way to handle an emergency is to prevent it from happening in the first place (awareness of potential dangers) and to have on hand some sort of first-aid kit, either in your vehicle or in your backpack. A reasonably good, basic first aid kit can be purchased for as little as $25 (St John First Aid Kit - Woolworths)
A Basic First Aid Kit should include the following:-
non-stick wound dressings
adhesive strips (e.g. Bandaids)
combine & eye pads
gauze swabs
alcohol & antiseptic swabs
triangular bandages
crepe bandages (including a purpose made snake bite bandage)
disposable hand towels
stainless steel scissors
blunt-nosed shears
saline solution
safety pins
plastic bags
stainless steel tweezers
thermo/shock blanket
notepad & pencil
disposable nitrile gloves
bite & itch relief gel
cold pack (disposable)
CPR protection mask
Additional products recommended are:-
antiseptic cream
laxatives
analgesic tablets
allergy preparations
anti-nausea preparations
anti-diarrhoea preparations
sunscreen, sunburn-relief
ear ache drops
eye drops
cotton buds
finger stalls
medicine measuring cup
thermometer
a blue asthma inhaler (if
permitted)
Check the contents of your kit regularly, and ensure that:-
items have been cleaned
packets are properly sealed
items have not exceeded expiry dates
previously used items have been replaced
1/ Physical Trauma - this includes injury from car/motorcycle/boat/bicycle/hang-glider accident; falls from and/or onto hard objects, such as rocks; Crocodile or Shark attack; other wild animal attacks, such as Feral Pigs; injury from a sharp object, such as a spear, sharp tree branch, sharp rock/coral, glass or metal object; electrocution; burns and scalds.
2/ Bites And Stings - this includes snake, spider, scorpion and centipede bites; jellyfish stings; Stingray, Stonefish, Bullrout and Coneshell barb stings.
3/ Medical Emergencies - this includes heart attack; stroke; convulsions/seizures; fainting or collapse; cessation of breathing (drowning etc.); anaphylaxis; involuntary bleeding; low or high blood sugar; heat stroke; dehydration; exposure; severe headache; accidental poisoning/drug overdose.
In any emergency the first response is to follow DRSABCD
Danger
Ensure the area is safe for yourself, others and the casualty
Response
Check for response - ask name - squeeze shoulders (Also look for any medical identifications, such as a necklace or a bracelet. This may provide a valuable clue to the cause of the situation)
No Response -> Call for help
Response -> Make comfortable, monitor response and check for injuries
Send
Call 000 for an ambulance or ask someone else to make the call
Send for a defibrillator if available
Airway
Open mouth - check for foreign material
No Foreign Material -> Leave casualty in the position in which they were found. Open the airway by tilting head with chinlift (adult) or slight head tilt and chinlift (child).
Foreign Material In Mouth -> Place casualty in the recovery position with mouth slightly downward. Clear foreign material from airway with fingers. Once foreign material is removed, open the airway with a head tilt and chin lift (adult) and slight head tilt and chin lift (child).
Breathing
Check for breathing. Look for movement of the upper abdomen or lower chest. Listen for the escape of air from the nose and mouth. Feel for movement of air at the mouth and nose.
Not breathing normally and no response -> Place on back and commence CPR and defibrillation.
Normal breathing -> Place in recovery position, monitor breathing and responsiveness.
CPR For Adult (For Child See Below)
->
Place the heel of hand on the lower half of the breastbone in centre of the chest with other hand on top of first. Either a one or two hand technique can be used for performing chest compressions in children.
-> Press down 1/3 of depth of chest and release, giving 30 compressions.
-> Open the casualty’s airway (head tilt and chin lift).
-> Pinch the soft part of the nose to seal and place your mouth over the casualty’s mouth.
-> Blow steadily into mouth for up to 1 second, watch for chest to rise and fall.
-> Give 2 breaths. Repeat 30 compressions to 2 breaths.
-> Aim for approximately 100-120 compressions per minute.
-> Continue CPR (30:2) until an ambulance arrives or casualty recovers.
Defibrillation
Turn ON the defibrillator as soon as possible (if available) and follow voice prompts
How to perform CPR -
Instructions And Diagrams (Adult)
Instructions And Diagrams (Child Under 12 Months)
Instructional Video
How To Place A Patient In The Recovery Position
Anaphylaxis -
A severe allergic reaction is the body’s immune system overreacting to a foreign substance. This is called Anaphylaxis and is potentially life-threatening.
Caused by:
- Food: Nuts, cow’s milk, eggs, fish, shellfish and soy products.
 - Medications: Penicillin, Sulphur, antibiotics, Aspirin, Ibuprofen, Codeine or Morphine.
- Medications: Penicillin, Sulphur, antibiotics, Aspirin, Ibuprofen, Codeine or Morphine.
- Venom: Bites from ticks, stings from bees, wasps and ants.
Signs and symptoms:
- Difficult and/or noisy breathing.
- Wheeze or persistent cough.
- Swelling of the face and tongue.
- Swelling/tightness of the throat.
- Difficulty talking and/or “hoarse” voice.
- Persistent dizziness or collapse.
- Young children may become pale and floppy.
- Abdominal pain and vomiting.
- Hives, welts and body redness.
What to do:
- Follow DRSABCD.
- Lay the casualty flat.
- If breathing is difficult allow them to sit.
- DO NOT allow them to stand or walk.
- If the casualty is carrying an adrenaline autoinjector, use it immediately.
- Ask the casualty if they need your help to use the adrenaline auto-injector.
- Urgent medical aid. Call Triple Zero (000) for an ambulance immediately.
If required assist the casualty with an adrenaline autoinjector.
(EpiPen®)
- Form a firm fist around the EpiPen® and pull off the BLUE SAFETY RELEASE.
- Place ORANGE END against outer mid-thigh at a 90° angle (can be injected through clothing).
- Push down hard until a click is heard or felt and hold in place for three (3) seconds.
- Remove EpiPen® and dispose of it safely being careful of the needle.
- Monitor the casualty, if no improvement, administer a second dose after 5 minutes.
(Anapen®)
- Pull off black needle shield.
- Pull off grey safety cap from red button.
- Place needle end firmly against outer mid-thigh at 90° angle (with or without clothing).
- Press red button so it clicks and hold for 3 seconds. Remove Anapen®.
- Monitor the patient. If there is no improvement after 5 minutes, use another adrenaline auto-injector, if available.
- Commence CPR and defibrillation at any time if the casualty is unconscious and is not breathing normally.
Anaphylaxis Action Plans At ASCIA
Arthropod Bites And Stings -
(Less dangerous arthropod species - not including spiders and scorpions)
Most insect bites and stings result in a localised itch and swelling that settles within a few days. Severe allergic reactions (anaphylaxis) from insects are usually due to bees, wasps or one of several ant species.
 Caused by:
Caused by:
- Bites or stings from an insect (bee, wasp, ant etc.), small arachnid (tick) or other arthropod (e.g. centipede)
Signs and symptoms:
- Pain at the site (sometimes extreme)
- Swelling and redness
- Muscle weakness (tick bite)
- Difficulty in breathing and swallowing
- Itchy and painful blisters
What to do:
- Follow DRSABCD
Bee/wasp sting - remove the sting by scraping sideways with fingernail or sharp object
Tick bite - if any signs of allergic reaction or casualty has a known allergy - DO NOT remove the tick
- If any signs of allergic reaction or casualty has a known allergy - the tick must be killed where it is rather than removed, if you have the appropriate equipment to do so. Use an ether-containing spray to kill the tick, or TeaTree Oil or Sodium Bicarbonate to encourage it to drop off. This should be performed in a safe place with medical aid
Centipede/Ant bite - wash bitten area thoroughly with soap and water
- Apply a cold pack directly over the bite site to relieve pain
- Monitor casualty and seek medical aid if necessary
- If severe allergic reaction, call 000 for an ambulance
- If the casualty is carrying their own adrenaline auto-injector (EpiPen®) it should be given immediately
- If there is no sign of allergic reaction, take pain medication: Paracetamol or ibuprofen can help with pain
Asthma Attack -
An asthma attack is a sudden worsening of asthma symptoms triggered by the tightening of muscles around the airways.
Triggers may include:
- Exercise/activity
- Respiratory infections
- Inhaled allergens, such as pollen
- Changes in temperature and weather, especially cold air.
- Environmental factors
- Emotional factors, such as anxiety, stress or laughter
- Certain medications e.g. aspirin
- Chemicals and strong smells
- Some foods and food preservatives.
Symptoms and signs of a severe asthma attack:
 - Dry, irritating, persistent cough
- Dry, irritating, persistent cough
- Gasping for breath
- Unable to speak more than one or two words per breath
- Blue discolouration around the lips
- Pale and sweaty skin
- Symptoms rapidly getting worse or using reliever more than every two hours.
What to do:
Conscious casualty -
- Follow DRSABCD.
- Sit the casualty comfortably upright.
- Be calm and reassuring and don’t leave the casualty alone.
- Help the casualty to take four (4) puffs from their inhaler following their Asthma Action Plan (if they have one).
- Wait four (4) minutes - if the casualty still cannot breathe normally, give four (4) more puffs in the same way.
- If the casualty gets little or no relief from the inhaler, call Triple Zero (000) for an ambulance.
- Keep giving four (4) puffs every four (4) minutes until medical aid arrives.
How to give Asthma medication:
With a spacer -
- Assemble spacer.
- Remove puffer cap and shake well
- Insert puffer upright into spacer
- Place mouthpiece between teeth and seal lips around it
- Press once firmly on puffer to fire one (1) puff into spacer
- Take four (4) breaths in and out of spacer
- Repeat one (1) puff at a time until four (4) puffs taken
- Remember to shake the puffer before each puff.
Without a spacer -
- Remove puffer cap and shake well
- Breathe out away from puffer
- Place mouthpiece between teeth and seal lips around it
- Press once firmly on puffer while breathing in slowly & deeply
- Slip puffer out of mouth
- Hold breath for four (4) seconds or as long as comfortable
- Breathe out slowly away from puffer
- Repeat one (1) puff at a time until four (4) puffs taken
- Remember to shake the puffer before each puff.
Unconscious casualty -
- Follow DRSABCD.
- If CPR is required it may be more difficult to get a breath into the casualty’s lungs
Bat Bite Or Scratch -
In Australia, flying foxes or other bats can carry lyssavirus (also known as ABLV: Australian bat lyssavirus) which is potentially fatal.
These animals must never be handled by people who are not trained to handle wildlife, even if the animal is injured.
 What to do:
What to do:
Anyone either bitten or scratched by a bat should IMMEDIATELY:
- wash the wound thoroughly with soap and water
- seek medical aid, regardless of the site or severity of the wound.
A protective vaccine can be administered even after the bite.
ABLV
Australian bat lyssavirus (ABLV), originally named Pteropid lyssavirus (PLV), is a enzootic virus closely related to the rabies virus. It was first identified in a 5-month-old juvenile black flying fox (Pteropus alecto) collected near Ballina in northern New South Wales, Australia, in January 1995 during a national surveillance program for the recently identified Hendra virus.
ABLV is the seventh member of the genus Lyssavirus (which includes Rabies virus) and the only Lyssavirus member present in Australia. ABLV has been categorized to the Phylogroup I of the Lyssaviruses.
Bats, both flying foxes and insectivorous bats, are the only known host reservoir for ABLV. The known species of bat reservoirs are the Black Flying Fox (Pteropus alecto), the Grey-headed Flying Fox (P. poliocephalus), the Spectacled Flying Fox (P. conscpicullatus), the Little Red Flying Fox (P. scapulatus), and the Yellow-bellied Sheathtail Bat (Saccolaimus flaviventris). These species are distributed throughout the Australian continent, and ABLV has only been serologically and phylogenetically detected in Australia.
It is estimated that less than 1% of healthy bats are ABLV carriers. As for sick or injured bats, it is estimated that 5-10% have been infected, detected with fluorescent antibody testing.
Due to its difficulty in diagnosing, low number of reported cases, and relative novelty as an endemic virus, there are no successful treatment plans once the symptoms have begun. All intervention methods used on the three known human cases of ABLV were not curative and all three cases resulted in fatality.
However, it is highly recommended by physicians to receive the RABV post-exposure prophylaxis (PEP) protocol immediately after potential lyssavirus exposure (i.e. exposure/interaction with bats). Additionally, the incident should be reported to the relevant public health unit. Currently, the PEP protocol involves thoroughly cleaning the wound and surrounding tissue, administration of the rabies vaccine, and administration of rabies immunoglobulin (RIG).
Blue-Ringed Octopus Bites And Cone Shell Stings (See further below for other "Marine Stings") -
The Greater Blue Ringed Octopus (Hapalochlaena lunulata) is commonly found in shallow tropical to sub-tropical waters, and if handled may inflict a potentially fatal bite. This may not be painful, as venom is not always injected.
The Cone Shell (Conus sp,) is mainly found in tropical waters; envenomation happens when they are handled or stepped on and they fire a dart-like barb which delivers venom.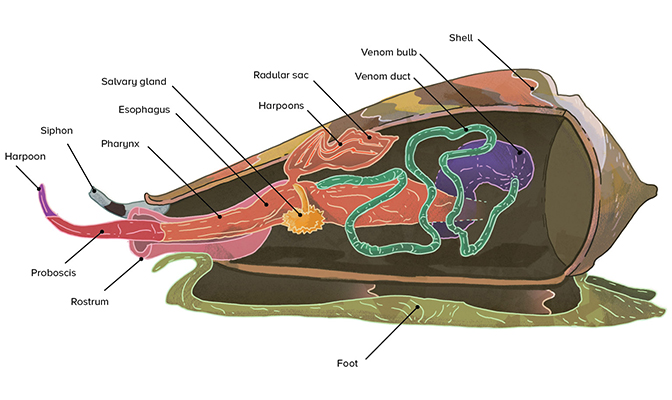
Although different, venoms from both these creatures can cause paralysis and death from respiratory failure within 30 minutes.
Please see the "Dangerous Fauna" page for details on these very dangerous marine creatures.
Signs and symptoms:
- A painless bite with a spot of blood visible
- Numbness to lips and tongue, muscle weakness of respiration which can stop the casualties breathing
Caused by:
- Handling the creature
- Accidentally standing on the creature
What to do:
- Follow DRSABCD
- Urgent medical aid. Call 000 for an ambulance
- Calm casualty and keep them still
- If the bite is on a limb apply a firm broad crepe or elasticised roller bandage starting just above the fingers or toes, and moving upwards on the bitten limb as far as can be reached and immobilise the limb with a splint
- Monitor casualty closely for signs of adverse reactions or deterioration
- Prepare to perform cardiopulmonary resuscitation (CPR) if necessary
Burns And Scalds -
Burns and scalds are damage to the skin caused by heat. A burn is caused by dry heat and a scald is caused by something wet and hot. Burns can also affect the respiratory system and the eyes.
Caused by:
- Heat (thermal)
 - Fire or radiant heat such as an electric cooker
- Fire or radiant heat such as an electric cooker
- Hot liquid and steam
- Radiation from the sun
- Chemicals - corrosive substances
- Electricity
- Friction, such as a rope burn.
Signs and symptoms:
Superficial burn -
- Skin is red and painful, may blister and swell.
Deep burn -
- Skin is white, dark red or charred
- No pain where nerve endings have been destroyed
- Usually surrounded by superficial burns.
What to do:
- Follow DRSABCD.
- If clothing is on fire: STOP-DROP-ROLL
+ Stop the casualty from moving around.
+ Drop the casualty to the ground and wrap in a blanket or similar.
+ Roll the casualty along the ground until flames are smothered.
- Assess the adequacy of the casualty’s airway and breathing.
- Cool the burnt area with copious amounts of cool (fresh) water for up to twenty (20) minutes.
- Remove any clothing and jewellery from affected area unless stuck to the burn.
- Cover burnt area with a light non-stick dressing or clean, dry non-fluffy material.
- Rest and reassure the casualty and check for shock.
Call Triple Zero (000) if:
+ Burns involving airway, hands, feet, face or genitals.
+ Deep burn.
+ Superficial burn larger than twenty (20) cent piece on an adult or ten (10) cent piece on a child.
+ If in any doubt of what to do.
DO NOT
- Peel off clothing that is stuck to the skin
- Use ice or iced water to cool a burn
- Apply lotions, ointments or creams
- Break blisters
Choking Adult or Child (Over 1 year old) -
Choking is severe difficulty when breathing due to a mild or severe obstruction of the airway due to a foreign body.
Caused by:
- Airway partially or completely blocked by food
 - Airway partially or completely blocked by small objects or foreign materials
- Airway partially or completely blocked by small objects or foreign materials
- Eating too quickly
- Not chewing food sufficiently.
Signs and symptoms:
- Clutching the throat
- Coughing, wheezing or gagging
- Having difficulty breathing, unable to breathe, coughing while speaking or swallowing
- Trying to cry but making strange or no sounds at all
- Making whistling or “crowing” sounds
- Face, neck, lips, ears or fingernails turning blue
- Collapsing or becoming unconscious.
What to do:
- Follow DRSABCD
- Encourage the casualty to relax, breathe deeply and encourage coughing to remove object and observe for any deterioration.
- If coughing is unsuccessful in removing the object, call Triple Zero (000) for an ambulance.
If the casualty is conscious -
- Position the casualty leaning forward with their head and chest low and give up to five (5) sharp back blows between the shoulder blades with the heel of one hand.
- Visually check after each back blow to see if the obstruction has been cleared.
- If unsuccessful, give up to five (5) chest thrusts:
+ Use the heel of the hand on the breastbone.
+ Place the other hand flat between the shoulder blades to support the casualty and deliver up to five (5) chest thrusts. Chest thrusts are similar to chest compressions but sharper and delivered at a slower rate.
+ Visually check to see if the obstruction has cleared after each thrust.
- If the obstruction does not clear, continue alternating with five (5) back blows and five (5) chest thrusts until medical aid arrives.
If the casualty becomes unconscious and is not breathing normally -
- Commence CPR and defibrillation
- Call Triple Zero (000) for an ambulance
Choking Infant (Under 12 months old)
Signs and symptoms: - clutching the throat
- clutching the throat
- coughing, wheezing, gagging
- difficulty in breathing, speaking or swallowing
- making a whistling or ‘crowing’ noise, or no sound at all
- blue lips, face, earlobes, fingernails
- loss of consciousness
What to do:
- Immediately call Triple Zero (000) for an ambulance.
Stay on the phone.
- Place the infant with their head downwards on your forearm, supporting the head and shoulders on your hand.
- Hold the infant’s mouth open with your fingers.
- Give up to 5 sharp blows to the back between the shoulders with the heel of one hand, checking if the blockage has been removed after each blow.
- If the blockage has come loose or been removed, turn the infant into the recovery position and remove any object that can have come loose with your little finger.
- If the blockage has not been removed after 5 back blows, place the infant on their back on a firm surface.
- Place 2 fingers on the lower half of the sternum and give up to 5 chest thrusts, checking if the blockage has been removed after each thrust. Support the infant’s head with the other hand.
- If the blockage has not been removed after 5 thrusts, continue alternating 5 back blows with 5 chest thrusts until medical aid arrives.
- If the infant becomes unconscious, start CPR.
Cold Induced Condition (Hypothermia) -
Cold-induced conditions occur when the body’s core temperature drops below 35ºC. The body’s natural reaction is to prevent body heat escaping and does this by shutting down blood vessels in the skin.
Caused by:
- Exposure to cold, wet, or windy conditions
 - Immersion/submersion in cold water
- Immersion/submersion in cold water
- Trauma, immobility and burns
- Severe infections
Signs and symptoms:
- Feeling cold, shivering
- Clumsiness and slurred speech
- Apathy and irrational behaviour
When body temperature drops very low:
- Shivering usually ceases
- Pulse may be difficult to find
- Heart rate may slow
- Level of consciousness continues to decline
- Unconsciousness
- Cardiac arrest may occur
What to do:
- Follow DRSABCD
- Move the patient to a warm, dry place
- Help the patient to lie down in a comfortable position. Handle the patient as gently as possible, avoiding excess activity and movement
- Remove any wet clothing from the patient
- Place the patient between blankets or in a sleeping bag, and wrap them in an emergency blanket
- Cover the patient’s head to maintain body heat
- Give the patient warm drinks if they are conscious. Do not give alcohol
- Place hot water bottles, heat packs and other sources of external heat directly on the patient’s neck, armpits and groin. Be careful to avoid burns. Body-to-body contact can be used if other means of rewarming are not available
- If hypothermia is severe, call Triple Zero (000) for an ambulance
- Stay with the patient until medical aid arrives.
DO NOT rub affected areas
DO NOT use radiant heat such as fire or electric heaters
DO NOT give alcohol
Concussion
Any person who has suffered loss of consciousness or an altered state of consciousness after a blow to the head should not return to their activity (eg sport) and should see a medical practitioner urgently.
Signs and symptoms: Some or all of the following can indicate concussion:
Some or all of the following can indicate concussion:
- loss of consciousness
- persistent headache
- faintness, dizziness
- confusion
- loss of memory, particularly of the event
- blurred vision
- slurred speech
- altered or abnormal responses to commands and touch
- vomiting within a few hours after a head injury
- wounds to the scalp or face
What to do:
- Follow DRSABCD
- If the patient is conscious and no spinal injury is suspected, place the patient in a position of comfort (usually lying down) with their head and shoulders slightly raised
- Advise them to seek medical attention
- If the patient is unconscious and a neck or spinal injury is suspected, place the patient in the recovery position, carefully supporting the patient’s head and neck, and avoid twisting or bending during movement
- Call Triple Zero (000) for an ambulance
- Ensure the patient’s airway is clear and open. Keep the patient’s airway open by lifting their chin. DO NOT force if the face is badly injured
Head injury:
- Control any bleeding with direct pressure at the point of bleeding. If you suspect the skull is fractured, use gentle pressure around the wound
- If blood or fluid comes from the ear, secure a sterile dressing lightly over the ear. Lie the patient on their injured side, if possible, to allow the fluid to drain
- Ensure an ambulance has been called, noting the patient’s condition so that you can report it to the paramedics.
Diabetic Emergency -
Diabetes is a condition where the body cannot maintain healthy levels of glucose, resulting in too much glucose in the blood. Glucose is a form of sugar which is the main source of energy for our bodies. Diabetic emergencies are when blood sugar levels become either too high or too low.
Caused by:
- Low blood glucose (Hypoglycaemia) - low blood glucose
- High blood glucose (Hyperglycaemia) - high blood glucose
Signs and symptoms:
Low blood glucose -
 - Hungry
- Hungry
- Pale, sweaty
- Weak or shaky
- May appear confused, irritable or aggressive
- Seizures
High blood glucose -
- Excessive thirst
- Frequent urination
- Hot, dry skin
- Feeling tired, blurred vision
- Fruity sweet smell of acetone on the breath
What to do:
- Follow DRSABCD
Conscious casualty -
Low blood glucose (Hypoglycemia) -
- Help casualty into a comfortable position and reassure them
- Give sugar such as glucose tablets, jellybeans or a sweet drink (such as a soft drink or cordial)
DO NOT give diet soft drinks or sugar-free cordials
- If the person is able to follow simple commands and swallow safely, administer 15-20 grams glucose tablets (4 - 5 x 4 gram glucose tablets)
- If symptoms or signs persist after 10 to15 minutes, and the person is still able to follow simple commands and swallow safely, administer a further 4 x 4g glucose
- Follow up with a sandwich or other food
- If there is no improvement call Triple Zero (000) for an ambulance
High Blood Glucose (Hyperglycemia) -
- Follow Diabetes Management Plan
- If the person has no management plan, seek medical assistance
Unconscious casualty -
- Call 000 for an ambulance
- Place the casualty into the recovery position if unconscious and not breathing normally
- Give nothing by mouth
Dislocation -
A dislocation occurs when one or more bones are displaced at a joint, this is most often at the shoulders, elbow, kneecap or fingers.
Caused by:
- A sudden impact on the joint
 - Forceful muscle contraction
- Forceful muscle contraction
Signs and symptoms:
- Pain at or near the site of injury
- Difficult or impossible to move the joint
- Loss of power
- Deformity or abnormal movement
- Tenderness
- Swelling
- Discolouration and bruising
What to do:
- Follow DRSABCD
- Assist the casualty to sit or lie down in a comfortable position and reassure
DO NOT attempt to put joint back into position
If the injury is to a limb:
+ Check blood flow - if absent move limb gently to try and restore it.
+ Call Triple Zero (000) for an ambulance.
+ Apply icepacks if possible, directly over the joint.
+ Rest and support the limb with padding and bandages
- Shoulder:
+ Support the casualties arm in position of least discomfort
- Wrist:
+ Apply a sling in a position of comfort
Dog Bite
See sections on:
- severe bleeding
- shock
Signs of wound infection:
- increased pain and soreness of the wound or wound area
- increased temperature (warmth) around the wound area
- increased swelling and redness of the wound and surrounding area
- pus oozing from the wound
- fever (if the infection persists)
- swelling and tenderness of the lymph glands
- tracking or red streaks leading away from the wound
What to do:
- Follow DRSABCD
- Wash and clean the wound with soap and water
- Apply a sterile dressing
- Monitor for signs of infection
- Seek medical aid if necessary
If the bite has resulted in a severely bleeding wound:
- Follow DRSABCD. Call Triple Zero (000) for an ambulance
- Apply gloves if available. Remove or cut the patient’s clothing to expose the wound
- Apply firm, direct and continuous pressure on the bleeding wound
– initially with your hands until the bleeding stops. The patient or a bystander can do this
- Apply a pad or dressing in or directly over the wound and apply firm, direct and continuous pressure until the bleeding stops
- Once bleeding is controlled secure the pad by bandaging firmly, ensuring the pad remains directly over the wound. Observe for any further bleeding
- Manage the patient for shock. Do not give the patient anything to eat or drink
- Continue to monitor the patient whilst waiting for medical aid
Drowning
Rescuing a drowning person:
The goal is to safely remove the drowning person from the water as soon as possible.
If you do not have the swimming abilities or strength to rescue the person from the water, attempt a ‘non-contact’ rescue technique such as reaching out with your hand or a sturdy stick, or throwing a float. At the same time,
shout for help and get another bystander to call
Triple Zero (000) for an ambulance. Providing oxygen:
Providing oxygen:
Following successful initial resuscitation, oxygen may be given if available and you are trained to do so.
What to do:
- Follow DRSABCD. Send for help
- Remove the drowning person from the water as soon as possible. Do not endanger your own safety
If the person is conscious:
- help the person to sit or lie down in a comfortable position and give reassurance
If the person is unconscious:
- assess the person on their back with their head and body at the same level
- assess the airway without rolling the casualty onto their side unless the airway is obstructed with fluid (water or blood) or matter (sand, debris, vomit). Clear any foreign matter from the airway
- if unresponsive and not breathing normally, start CPR
- If vomiting or regurgitation occurs during CPR, roll the person onto their side to clear the airway and reassess for signs of life. If breathing normally, leave the person on their side and monitor closely. If unresponsive and not breathing normally, roll the person onto their back and recommence CPR
- Avoid delays or interruptions to CPR. Do not empty a distended stomach by applying external pressure. It is not necessary to drain clear water or frothy fluid that can build up in the upper airway during CPR
- People who appear to have been successfully rescued and resuscitated need to be closely monitored. They should be referred for medical assessment
- Call Triple Zero (000) for an ambulance for all drowning casualties, even if the event is seemingly minor
Electric Shock/Lightning Strike -
An electric shock occurs when a person comes into contact with an electrical energy source. Electrical energy flows through a portion of the body causing a shock. Exposure to electrical energy may result in a life-threatening situation as there may be damage to internal organs.
Caused by:
- Electricity (either high voltage or prolonged current) passing through the body
- Lightning strike
Signs and symptoms:
- Sudden collapse after touching anything electrical
- Burns, particularly entry and exit burns where the electricity entered and left the body which may be deep
- Unconsciousness
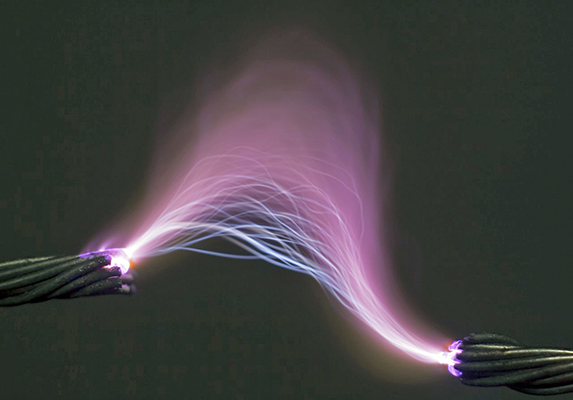 - Not breathing normally
- Not breathing normally
- A weak, erratic pulse or no pulse at all
- Cardiac arrest
What to do:
- Follow DRSABCD
- Check for danger to yourself and bystanders
- Switch off the power if possible
- If safe to do so, remove the casualty from the electrical supply without directly touching them
- Use non-conductive, dry materials, for example, a dry wooden broom handle
- Cool any burnt areas with copious amounts of cool water for up to 20 minutes
- Remove any clothing and jewellery from the affected area unless stuck to the burn
- Cover burnt area with a light non-stick dressing or clean, dry non-fluffy material
- Reassure the casualty
- Always seek medical aid immediately for electrical burns
- Call 000 for an ambulance
Downed power lines:
- When calling 000, advise that there are downed cables
- Phone Ergon Energy on 13 22 96 to report a fallen powerline and to make the area safe
- Remain at least 8 metres from any cable and do not approach until advised that it is safe to do so
DO NOT attempt to remove the cable
- If a vehicle is being touched by a high voltage cable, DO NOT go near the vehicle or try to remove the casualty from the vehicle
- Advise the casualty not to move
Eye Injuries -
The eyes are the most sensitive and delicate organs in the body and are easily injured. An eye injury is a trauma or damage to the eye caused by a direct blow to the eye.
Caused by:
- Impact with objects, such as a fist, ball, stones or tree branches
- Small foreign objects, such as dirt, slivers of wood/metal or sand
- Chemicals, such as acid, caustic soda, lime
 - Flames, flash burns, smoke or lasers
- Flames, flash burns, smoke or lasers
Signs and symptoms:
- Pain
- Redness
- Photophobia - abnormal visual intolerance to light
- Watering or bleeding
- Pupil distortion, impaired vision
What to do:
- Follow DRSABCD
- Act with extreme urgency (within seconds) if it is a heat or chemical burn
- Wash hands thoroughly and wear gloves if available
DO NOT -
Touch the eyeball or any contact lens;
allow the casualty to rub their eye;
try to remove any object which is penetrating the eye; apply pressure when bandaging the eye.
Minor injury -
- Wash out the eye gently with water or normal saline, from the corner closest to the nose outwards
- If unsuccessful, pad eye and seek medical aid
Major injury -
DO NOT remove any embedded object.
- Lay casualty flat on their back and reassure
- If a penetrating eye injury - carefully place pads around the object and bandage gently in place
DO NOT place pressure on the eye.
- Pad the head on each side with blankets/towels to stop the casualty from moving their head
- Reassure casualty and ask them to keep their head as still as possible, as they will be anxious
- Urgent medical aid. Call 000 for an ambulance
Fainting (Syncope)
Fainting is a partial or complete loss of consciousness caused by a temporary reduction of blood flow to the brain.
People usually recover from fainting quickly, often within seconds, without any lasting effects.
Signs and symptoms:
 - pale, cool, moist skin
- pale, cool, moist skin
- numbness in the fingers and toes
- nausea
- faintness, dizziness
- confusion
- loss of consciousness
Fainting can occur at any time and can be triggered by:
- emotional shock
- pain
- overexertion
- exhaustion
- lack of food
- sight of blood
- low blood pressure
- standing still in hot conditions
What to do:
- Follow DRSABCD
- Lie the patient down on their back with their legs elevated
- Loosen any tight clothing
- Ensure plenty of fresh air, open a window if possible
- Treat any injury resulting from a fall
- If fainting is the result of an underlying medical condition, advise the patient to seek medical aid
DO NOT
- sit the patient on a chair with their head between their knees
Febrile Convulsions -
A Febrile Convulsion is a fit or a seizure that occurs in children aged 6 months to 5 years. Convulsions in infants and children are quite common and usually brief, lasting no more than 5 minutes.
Caused by:
- A rapid rise in body temperature to even 1.5ºC above the norm (37.5ºC) can cause convulsions
- Fever
 - Infection
- Infection
- Other conditions
Signs and symptoms:
- Fever (can be as low as 38.5°C)
- Muscle stiffening
- Twitching or limb jerking
- Eyes rolling upwards
- Blue tinge to face and lips
- Unconsciousness
What to do:
During convulsion -
- Follow DRSABCD
- Place the child/infant on their side
- DO NOT restrain the child/infant.
- Remove child’s excess clothing or wrapping to cool them down - DO NOT cool by sponging or bathing
After convulsion -
- Follow DRSABCD
- Place infant/child into the recovery position if unconscious and breathing
- Rest and reassure
- Monitor airway and breathing, and keep cool
- Seek medical aid
If the casualty’s temperature rises again or another seizure follows - call 000 for an ambulance
Fractures (Broken Bones) -
A fracture is a broken bone. It can be difficult to tell whether the injury is a fracture, dislocation, sprain or strain. If in doubt, always treat as a fracture.
Caused by:
- Direct force, at site of impact
 - Indirect forces e.g. fall on feet and break spinal bone
- Indirect forces e.g. fall on feet and break spinal bone
Signs and symptoms:
- Pain at or near the site of the injury
- Difficult or impossible normal movement
- Loss of function
- Deformity or abnormal mobility
- Tenderness and swelling
- Discolouration and bruising
- Broken bone penetrating skin and bleeding
Types of Fractures:
Closed - Bone is broken with skin intact
Open - Broken bone protrudes through skin or there is a wound
Complicated - Associated injury to a major nerve, blood vessel, or vital organ(s)
What to do:
- Follow DRSABCD
- Control any bleeding and cover any wounds
- Rest and reassure, ask the casualty to remain still
- Immobilise the fracture in most comfortable position
DO NOT attempt to force a fracture back into place
- Use broad bandages (where possible) to immobilise the fracture
- Place a padded splint along the injured limb then bandage above and below the fracture site leaving a 5 cm gap either side of the fracture to prevent movement
DO NOT bandage over the fracture.
- The casualty may be able to support the fracture themselves
- Check that bandages are not too tight or too loose and every 15 minutes watch for signs of loss of circulation to hands or feet
- Seek medical aid or call 000 for an ambulance if required
Head Injuries -
Head injuries are the result of trauma to the skull, scalp or brain. Injuries to the head are potentially dangerous and always require medical attention.
Caused by:
Skull fracture from direct force e.g. blow to the head or indirect force e.g. a fall from height
Concussion - altered state of consciousness
Compression - excess pressure on part of the brain
Signs and symptoms:
 - Change in conscious level
- Change in conscious level
- Headache, nausea, vomiting
- Loss of memory
- Altered or abnormal responses to commands or touch, such as irritability, confusion
- Twitching, noisy breathing
- Wounds to the scalp or face
- Blood or fluid from the ear
- Dizziness
- Blurred vision
What to do:
Conscious casualty -
- Follow DRSABCD
Rest and reassure the casualty
- If NO suspected neck or spinal injury, place casualty in a comfortable position with head and shoulders slightly raised
- If neck or spinal injuries are suspected, protect the neck whilst maintaining a clear airway, keep the casualty flat and support the head on either side to stop movement; improvise using rolled towels, blankets or clothing
- Observe for any changes in signs, symptoms and level of consciousness
- Urgent medical aid. Call 000 for an ambulance
Unconscious casualty -
- Follow DRSABCD
- Urgent medical aid. Call 000 for an ambulance
- Place the casualty into the recovery position being careful to support the casualty’s head and neck in neutral alignment during movement to avoid any twisting action
- If any blood or fluid is coming from the ear, place injured side down to allow the fluid to drain, place a clean pad between ear and ground and observe the amount draining
- Monitor for any changes in signs, symptoms and level of consciousness and ensure the airway is kept clear and open
- Control any bleeding, but do not apply direct pressure to the skull
Heart Attack -
A heart attack is a pain caused by a blockage of an artery that supplies blood to the heart and causes damage or death of the heart muscle.
Caused by:
- Narrowing of the arteries
- A diet high in saturated fats
- Smoking
- High blood pressure
Signs and symptoms:
The warning signs of heart attack vary.
Symptoms can start suddenly or develop over time and get progressively worse. People may have just one symptom or a combination of symptoms.
The patient may feel discomfort or pain in the centre of the chest.
This pain may: - start suddenly, or start slowly over minutes
- start suddenly, or start slowly over minutes
- be described as tightness, heaviness, fullness or squeezing
- be severe, moderate or mild
- spread to the neck and throat, jaw, shoulders, the back, and one or both arms.
Atypical signs and symptoms:
However, not all patients define their pain as a
heaviness or squeezing.
The patient may also:
- feel short of breath
- have a choking feeling in the throat
- feel that their arms are ‘heavy’ and ‘useless'
- feel nauseous
- have a cold sweat
- feel faint or dizzy.
Only minimal symptoms may be described by women, the elderly, people with diabetes or chronic inflammatory conditions, Aboriginal
and Torres Strait Islanders, Māori and Pacific Islanders.
Symptoms may be only:
- breathlessness
- nausea
- arm or jaw pain.
What to do:
Conscious casualty -
- Follow DRSABCD
- Locate the nearest defibrillator and keep it on standby
- Advise the casualty to immediately sit down to rest and reassure them
- If the casualty has been prescribed medication such as a tablet or oral spray for angina, assist them to take it as they have been directed
- If symptoms last for 10 minutes or become worse quickly or are severe, call 000 for an ambulance immediately
- Give 300mg (one tablet) of aspirin with water
- DO NOT give aspirin to those allergic to it or if their doctor has advised them against taking aspirin
- Stay with the casualty and monitor consciousness and vital signs
- Be prepared to give CPR and administer defibrillation if symptoms worsen
Unconscious casualty -
- Follow DRSABCD
- Locate the nearest defibrillator and keep it on standby
- Place casualty in recovery position
- Urgent medical aid. Call 000 for an ambulance
- Stay with the casualty and monitor breathing
- Be prepared to give CPR and administer defibrillation if symptoms worsen
Heat Induced Condition (Hyperthermia) -
Heat-induced conditions occur when the body’s core temperature is elevated. This is known as Hyperthermia.
Caused by:
- Excessive heat absorption from a hot environment
- Excessive heat production from metabolic activity
- Failure of the body’s cooling mechanisms
 - An alteration in the body’s set temperature
- An alteration in the body’s set temperature
Signs and symptoms:
- Inability to continue the activity
- High body temperature
- Dizziness and faintness
- Nausea, vomiting or diarrhoea
- Pale skin and other signs of shock
- Dry skin
- Poor muscle control or weakness
- Decreasing levels of consciousness
- Confusion or seizures
What to do:
- Follow DRSABCD
Cooling management -
- Lie the person in a cool environment or in the shade
- Loosen and remove excessive clothing
- Send for an ambulance if not improving quickly
While waiting for professional assistance for individuals over 5 years of age -
- Immerse (i.e. whole-body from the neck down) in cold water (a bath if possible, as cold as possible) for 15 minutes
If this is not available, a combination of the following methods should be used -
- Wet the person with cold or cool water, under a shower if safe, or with a hose or other water source
- Apply ice packs (groin, armpits, facial cheeks, palms and soles)
- Repeatedly moisten the skin with a moist cloth or water spray
- Fan continuously
- While waiting for professional assistance for children 5 years of age and under -
- Cool in a tepid (lukewarm) bath sponging frequently if bath available, or -
- Repeatedly moisten the skin with a moist cloth or atomizer spray
- Fan continuously
Hydration Management -
- Give cool or cold water to drink if fully conscious and able to swallow
Jellyfish Stings (Tropical) -
The Box Jellyfish (Chironex fleckeri) and the Irukandji Jellyfish (Malo kingi and Carukia barnesi) are found in tropical waters that range from Geraldton, across the north, to Agnes Waters.
The Box Jellyfish are large, cube-shaped and have tentacles (up to 3m long) draping from the body which produce very potent venom. The stings from these are painful and can be fatal to humans
The Irukandji are small jellyfish and at times too small to be seen. The sting can be minor but can cause severe generalised pain and rarely death.
Please see the "Dangerous Fauna" page for details on these highly dangerous jellyfish.
Caused by:
- Contact with jellyfish tentacles
Signs and symptoms:
- Pain at the site (sometimes extreme)
- Respiratory and cardiac arrest sometimes within minutes (Box Jellyfish)
- Severe pain (back and abdomen)
- Nausea
- Vomiting
- Sweating
- Feeling of impending doom (Irukandji)
What to do:
- Follow DRSABCD
- Remove casualty from the water
- Urgent medical aid. Call 000 for an ambulance
- Calm casualty
- Flood stung area with vinegar for at least 30 seconds
- If vinegar is unavailable, flick tentacles off using a stick or gloved fingers and rinse with seawater
DO NOT use freshwater, this will cause further stinging cell discharge
- Apply a cold pack
- Rest and reassure, monitor vital signs and consciousness until medical aid arrives
- Give CPR if necessary
Leeches -
Leeches are segmented worms in the Subclass Hirudinea that are usually ectoparasitic. They are bilaterally symmetrical, with thick muscular bodies. Usually they are dorso-ventrally (front to back) flattened and segmented, though the segments are not often seen. Some leeches are long and worm-like, others pear-shaped and broad. Most can vary considerably in shape both between the elongated and contracted state and between the starved and full condition. The body tapers towards the head and has a small oral sucker surrounding the mouth and a larger caudal (tail) sucker at the rear end, except the marine fish parasites, Pisciolidae, which have a larger oral sucker. The anus is on the dorsal surface (top) just in front of the rear sucker.
Leeches usually have three jaws and make a Y-shaped incision. The Australian land leech has only two jaws and makes a V-shaped incision. Contrary to information commonly posted online, the most common leech encountered in the Wet Tropics is not "Gnatbobdellida libbata". This is, at best, a mis-spelling of an early alternative name for Chtonobdella limbata (Old Synonym - Gnathobdellida limbata). See "Dangerous Fauna" for a list of commonly encountered leeches in FNQ.
Where you will find them:
Most leeches are freshwater animals, but many terrestrial and marine species occur. Land leeches are common on the ground or in low foliage in wet rain forests. In drier forests they may be found on the ground in seepage moistened places. Most do not enter water and cannot swim, but can survive periods of immersion.
In dry weather, some species burrow in the soil where they can survive for many months even in a total lack of environmental water. In these conditions the body is contracted dry and rigid, the suckers not distinguishable, and the skin completely dry. Within ten minutes of sprinkling with a few drops of water, these leeches emerge, fully active.
Freshwater leeches prefer to live in still or slowly flowing waters, but specimens have been collected from fast flowing streams. Some species are considered amphibious as they have been observed in both terrestrial and aquatic habitats.
Leeches can be found almost anywhere in Australia where there are suitable damp areas and watercourses although they are absent from the permanently arid areas.
What leeches eat:
Leeches feed as blood sucking parasites on preferred hosts. If the preferred food is not available most leeches will feed on other classes of host. Some feed on the blood of humans and other mammals, while others parasitise fish, frogs, turtles or birds. Some leeches will even take a meal from other sanguivorous leeches which may die after the attack.
Are leeches dangerous:
The presence of hirudin in the wound following a leech bite may cause oozing to continue for several hours. Although inconvenient, blood loss is not significant. Their gut bacteria can cause wound infection. There may also be a delayed irritation and itching after a bite. There appears to be no support for the theory that mouthparts left behind after forced removal of the leech causes this reaction.
Can leeches transmit disease:
There is no evidence to suggest that they do. The presence of trypanosomes in the gut of jawless leeches has been noted, but jawed leeches do not appear to be hosts. Trypanosomes cause the African sleeping sickness in humans. Leeches transmit trypanosomes that infect fish, crocodiles and even platypus, but none of them are dangerous to humans. Allergy to leech bite has been reported. Medical opinion should be sought, depending on the severity of the reaction.
The biggest problems occur with people who are allergic to the bite, or when a leech bite remains untreated for several hours after the leech has been removed. This latter condition can lead to infection at the wound site, or even blood poisoning.
How to keep leeches away:
- Wear protective clothing: Leeches can’t bite through thick and tight-fitting clothing, so wearing long-sleeved shirts and pants can help protect your skin.
- Use a natural repellent: Applying a natural repellent (such as Oil of Lemon Eucalyptus) on your skin won’t harm leeches and can help keep them away.
- Avoid areas with standing water: Leeches are often found in damp areas, so try to avoid walking near standing water or wet vegetation.
- Use salt: Sprinkling salt on the ground around you (or on your clothing) can deter leeches as they do not like salt.
- Check your body regularly: If you are in an area where leeches are prevalent, make sure to check your body regularly for any attached leeches. The sooner you remove them, the less blood they will have ingested, and the less risk of infection.
It’s important to note that leeches are not harmful to humans in most cases, and they can even be used in medical treatments. However, if you are concerned about leech bites or have any other health concerns, it’s best to consult with a medical professional.
How to safely remove a leech:
Your first step in removing a leech is finding it. If you spot a leech on your skin, check the rest of your body to see if any more have attached themselves to you. Once you find a leech, you can begin to safely remove it.
The basic leech removal steps are:
- Locate the head and mouth. A leech’s head is smaller and slimmer than the rest of its body. Look for the narrowest part of the leech to locate its mouth. This is usually the part attached to your skin.
- Pull the skin under the leech taut. Use one hand to gently pull your skin under the leech until it’s taut.
- Slide a fingernail underneath the mouth. Gently slide a fingernail under the leech’s mouth to separate it from your skin.
- Flick the leech away. Use your fingers to flick the leech away before it reattaches.
- Clean the wound. Clean your wound with rubbing alcohol (Iso-Propyl Alcohol) or a first-aid cleanser to help avoid infection.
- Bandage your wound. You’ll see a lot of bleeding when you remove the leech. Clean the wound and then use a sterile bandage to cover it.
- Change the bandage frequently for the first few hours until bleeding stops.
Alternative methods for removing a leech:
- Using a piece of paper or a credit card instead of your fingernail. For this method, you’ll follow all the same steps as above, but you’ll slide a thin piece of paper or a credit card under the leech’s mouth instead of your finger.
- Letting the leech fall off naturally. Usually, this can take about 30-45 minutes. You can wait for the leech to detach itself when it’s finished feeding, especially if you’re having trouble removing it. If the leech does not fall off for a long time or attaches to a hard to reach area, having it medically removed is the best course of action.
Removing leeches from difficult locations:
Leeches will sometimes attach to hard-to-reach areas, like your ear canal, nose, eyes or mouth. This can make it difficult to use the above methods for removal. If this happens, try one or more of the following:
- Use rubbing alcohol (Iso-Propyl Alcohol) or hydrogen peroxide. To remove a leech from your mouth, gargle with alcohol or hydrogen peroxide for about 30 seconds. Swish the alcohol or peroxide in your mouth like mouthwash, then spit it out. Check to see if the leech comes out with it.
- Puncture the leech. Leeches can grow up to 10 times their original size when they’re feeding. Sometimes, this can cause them to block an area like your nose or ear. Use a sharp object to pop the leech, killing it and making it easier to remove.
- In some cases, the removal method will depend on the location the leech attaches to and may need the help of a medical professional to remove (e.g. the eye). Leeches that attach internally may require surgery to remove. This can happen if a person swallows contaminated water.
What NOT to do:
Do not remove a leech using any of the following methods. These can cause the leech to vomit blood into your wound and increase your risk of infection:
- salting
- fire
- shampoo
- bug repellant
- pulling the leech
Marine Stings (See further above for "Blue-Ringed Octopus Bites And Cone Snail Stings") -
Creatures such as the Striped Catfish (Plotosus lineatus), Stonefish (Synanceia sp), Bullrout (Notesthes robusta), Lionfish (Pterois sp.) and Crown-Of-Thorns Starfish (Acanthaster planci) can sting (penetrate) the skin via spines or barbs, which contain toxic material.
Stingrays have a whip-like tail which releases venom into the wound as it penetrates the skin. Many of these creatures can cause death.
Please see the "Dangerous Fauna" page for details of these dangerous marine creatures.
Caused by:
 - Spines or barbs penetrating the skin
- Spines or barbs penetrating the skin
Signs and symptoms:
- Immediate pain usually lasting 30 minutes
- Redness on the skin
- Muscle pain
- Nausea and vomiting
- Bleeding from the wound
- Breathing difficulties
- Cardiac arrest
What to do:
Catfish, Stonefish, Bullrout, LionFish, Crown-Of-Thorns Starfish -
- Urgent medical aid. Call 000 for an ambulance
- Follow DRSABCD
- Rest and reassure the casualty
- If the wound is on a limb, carefully remove any remaining spines or barbs. Clean visible foreign material from the wound.
If possible place the stung area in hot water (no hotter than the first aider can tolerate)
Stingray -
- Urgent medical aid. Call 000 for an ambulance
- Follow DRSABCD
- Rest and reassure the casualty
- Stop any severe bleeding before placing stung part in hot water (no hotter than the first aider can tolerate)
- DO NOT remove the embedded stingray spines especially from an injury to the chest, abdomen, neck, head, groin, or bone
Nosebleed Many nosebleeds do not have an obvious cause, but some can be because of:
Many nosebleeds do not have an obvious cause, but some can be because of:
- a blow to the nose
- excessive blowing
- sneezing
- high blood pressure
- changes to altitude
- prolonged exposure to high temperatures
Most nosebleeds will stop spontaneously or after simple treatment. Seek medical aid if the nosebleed persists or if the patient has frequent nosebleeds.
What to do:
- Ask the patient to breathe through their mouth and not to blow their nose. Encourage the patient to spit out blood rather than swallow it
- Help the patient to sit down with their head slightly forward
- Pinch the soft part of the patient’s nostrils, just below the bridge of the nose, for at least 10 minutes
- Loosen any tight clothing around the patient’s neck
- If bleeding persists, seek medical aid
Placing a cold pack on the patient’s neck and forehead might help the bleed. A cold pack is unlikely to cause any harm.
Poisoning -
Poisoning is a process of inhalation, ingestion, absorption, or injection of a poisonous substance.
Poisoning may be accidental or intentional and can occur from many different forms such as chemicals, alcohol, drugs, common plants, household items.
Please see the "Dangerous Flora" page for details of poisonous plants in the Greater Wangetti Region.
Caused by:
- Toxic fumes
- Toxic substances
- Bites and stings
Signs and symptoms:
Signs and symptoms depend on the type of poison, and can include:
- Confusion, drowsiness, delirium, seizures, unconsciousness
- bite or injection marks, with or without local swelling
- burns around and inside the mouth or on the tongue
- smell of fumes
- odours on the breath
- burning pain from mouth to stomach
- nausea, vomiting
- abdominal pain
- difficulty in breathing
- tight feeling in chest
- headache
- ringing in ears
- blurred vision
- blue lips, face, earlobes, fingernails
- drowsiness
- loss of consciousness
- seizures
- stroke
What to do:
- Follow DRSABCD
- Urgent medical aid is required. Call 000 for an ambulance
- Call Poisons Information 13 11 26 and/or follow instructions on any containers
- Send any vomit, containers, or notes with the casualty to the hospital
Conscious casualty -
- Listen to the casualty and give reassurance
- Find out what sort of poison is involved and keep any containers for the medical aid to see
- DO NOT induce vomiting or give anything to eat or drink
- Wash any corrosive substance off the mouth and face with water, or wipe off
Unconscious casualty -
- Place the casualty in the recovery position if unconscious and breathing and continue to check their airway and breathing regularly
Inhaled Poisons -
- Move casualty and yourself to fresh air
- Loosen tight clothing
Absorbed Poisons -
- Protect yourself (if possible) use protective clothing such as gloves, goggles, and so on
- Wash the substance off immediately
- Ask the casualty to remove any contaminated clothing
- Flush the casualty’s skin with running water
- Wash gently with soap and water and rinse well
Injected -
- Follow DRSABCD - avoid needle stick injuries to yourself and casualty
- Treat any other signs and symptoms. Send any empty syringes, bottles, and vials with the casualty to the hospital

Seizures And Epilepsy -
A seizure is a sudden surge of electrical activity in the brain. Seizures may vary from muscle jerks through to severe and prolonged convulsions. Epilepsy is a neurological disorder which triggers recurrent and unprovoked seizures. Not all seizures are epilepsy, but all require first aid.
Caused by:
- Head injury or high fever
- Brain tumour or stroke
- Poisoning or drug overdose
- Serious infection or lack of oxygen
- Epilepsy
Signs and symptoms:
- Sudden spasm of muscles producing stiffness or rhythmic jerking movements. If standing, the casualty will fall which may result in injury
- Suddenly cries out
- Shallow breathing or breathing may temporarily stop, leading to pale, blue-tinged lips and face
- Excessive saliva (frothing) from the mouth
- Changes in conscious state from being fully alert to confused, drowsy or loss of consciousness
What to do:
During a seizure -
- Follow DRSABCD and follow the casualty’s seizure management plan, if there is one in place
- DO NOT - Restrain the casualty or restrict movement.
Put anything in the casualty’s mouth.
Move the casualty, unless in danger.
- Protect casualty from environment: move furniture, cushion head and shoulders
- Ensure the airway is maintained
- Follow the casualty’s Seizure Management Plan if in place
- Record the duration of the seizure
After a seizure -
- Place casualty into Recovery Position if unconscious and breathing normally, ensure that the airway is clear and open
- Manage any injuries. Rest and reassure
- Seek medical aid
- DO NOT disturb if casualty falls asleep, but continue to monitor breathing and response
Call 000 for an ambulance if -
- First ever seizure
- The seizure continues for more than 5 minutes or another seizure quickly follows
- The casualty has been injured, is a diabetic or is pregnant
- The seizure occurs in water
Severe Bleeding -
Severe bleeding is an excessive amount of blood loss. Even a small injury can result in severe external bleeding, depending on where it is on the body.
Bleeding should be managed as severe and life-threatening if it cannot be controlled by firm, direct and continuous pressure, and/or there are signs of shock.
If it is obvious that severe and life-threatening bleeding is present, controlling bleeding before the Airway and Breathing can be life-saving. Send for help early by calling Triple Zero (000)
Caused by:
- Anything that cuts or damages a blood vessel (including Crocodile or Shark attack)
- Injury to a blood vessel
- Amputation of a body part
Signs and symptoms:
- Visible blood loss, oozing, flowing or spurting
- Pain
- Tenderness
- Feeling faint or dizzy
- Looking pale
- Thirsty
- Progressive loss of consciousness
What to do:
IMPORTANT wear gloves to prevent infection, if possible
Conscious casualty -
- Follow DRSABCD
- Reassure and lie the casualty down and remove or cut their clothing to expose the wound
- Apply direct pressure over and around the wound using a pad or your hands. If the injury is to a major artery, PUSH HARD, DON'T STOP
- Instruct the casualty to do this if possible
- Squeeze the wound edges together if possible
- Raise and support the injured part above the level of the casualty’s heart
- Handle gently if you suspect a broken bone
- Apply a pad over the wound and secure by bandaging over the wound
- If blood oozes through the original bandage do not remove it
- Place another pad and bandage over the top of the original one
- Monitor bleeding and check every 15 minutes that the bandages are not too tight and that there is circulation below the wound
If the bleeding is not controlled and:
- the bleeding is on a limb, apply an arterial tourniquet (if available) and tighten until the bleeding stops. Advise the patient that this will cause pai
- the bleeding is not on a limb, remove existing dressings and apply a haemostatic dressing (if available) in or directly over the wound and apply firm, direct and continuous pressure until the bleeding stops.
- Urgent medical aid. Call 000 for an ambulance
- DO NOT give the casualty anything to eat or drink
Unconscious casualty -
- Follow DRSABCD and follow the casualty’s seizure management plan, if there is one in place
- Control bleeding as for a conscious casualty
- Urgent medical aid. Call 000 for an ambulance
Shock -
Shock is a collapse of the circulatory system which results in insufficient oxygen reaching the vital organs and tissues. Shock can be life-threatening.
Caused by:
- Heart attack
- Bleeding
- Vomiting and diarrhoea
- Burns
- Pain or trauma
- Major or multiple fractures
- Infections
- Allergic reactions
- Severe sweating and dehydration
Signs and symptoms:
Initial shock:
- pale face, fingernails and lips
- cool, moist skin
- faintness, dizziness
- nausea
- anxiety
Severe shock:
- restlessness
- thirst
- weak, rapid pulse, which can become weaker or slower
- shallow, fast breathing
- drowsiness, confusion
- blue lips, face, earlobes, fingernails (this is a late sign and means the patient is very sick)
- unconsciousness
What to do:
Conscious casualty -
- Lie the casualty down with head flat on the floor and reassure
- DO NOT raise their legs
- Manage any other injury such as bleeding, wounds, burns and immobilise fractures
- Maintain the casualty’s body warmth. Cover with blanket, coat or similar but DO NOT use any source of direct heat
- Loosen any tight clothing
- If the casualty is likely to require any surgery DO NOT give anything by mouth. Otherwise offer clear fluids e.g. small amounts of water frequently
- Monitor the casualty
- DO NOT leave them alone
Unconscious casualty -
- Follow DRSABCD
- Place casualty into the Recovery Position if they become unconscious and are breathing normally
- Urgent medical aid. Call 000 for an ambulance
Snake Bite -
Snake bites are not common in Australia, but all should be treated as life threatening. Snakes force venom out under pressure through fangs in the upper jaw. The spread of snake venom depends on its absorption through the lymphatic system.
North Queensland has a smorgasbord of deadly snakes, fortunately death from a snake bite in the Greater Wangetti Region is extremely rare.
Please see the "Dangerous Fauna" page for a full list of life threatening snake species. Most commonly encountered are the Coastal Taipan, Death Adder, King Brown and Eastern Brown.
Caused by:
Snake fangs puncturing the skin and injecting toxin
 Signs and symptoms:
Signs and symptoms:
Signs of a snake bite are not always visible. In some cases, the patient may not have felt anything. Symptoms may not appear for an hour or more after the person has been bitten
Depending on the type of snake, signs and symptoms can include some or all of the following:
- immediate or delayed pain at the bite site
- swelling, bruising or local bleeding
- bite marks (usually on a limb) that can vary from obvious puncture wounds to scratches that can be almost invisible
- swollen and tender glands in the groin or armpit of the bitten limb
- faintness, dizziness
- nausea and vomiting
- headache
- abdominal pain
- oozing of blood from the bite site or gums
- double or blurred vision
- drooping eyelids
- difficulty in speaking or swallowing
- limb weakness or paralysis
- difficulty in breathing
- occasionally, initial collapse or confusion followed by partial or complete recovery.
What to do:
- Follow DRSABCD. Urgent medical aid. Call 000 for an ambulance
- Ensure the casualty does not move
- Lay the casualty down, rest and reassure
- If the bite is on a limb, apply a broad pressure bandage over the bite site as soon as possible
Then apply a further elasticised or firm bandage - start at fingers or toes and move up the limb as far as can be reached
Apply tightly but without stopping blood flow
- Splint the limb including the joints on either side of the bite
- Write down the time that the casualty was bitten and when the bandage was applied
- If the casualty becomes unconscious and not breathing normally, commence CPR and Defibrillation
DO NOT
- Wash the venom off the skin (it may aid in identification)
- Cut the bitten area and try to suck the venom out of the wound
- Use a tourniquet
- Try to catch the snake
Spider Bite/Scorpion Sting -
There are many species of spider that can, and sometimes will, bite a human but fortunately most are relatively harmless. In the Greater Wangetti Region we have two species that are potentially life threatening, and several others that can cause severe reactions. Scorpions are considered non-life threatening.
Hadronyche anzses - North Queensland Funnel-Web (potentially life threatening)
Latrodectus hasseltii - RedBack Spider (potentially life threatening to at least a child)
Please see the "Dangerous Fauna" page for a full list of dangerous spiders.
Caused by:
- Spider biting and puncturing the skin
- Scorpion sting from tail
Signs and symptoms:
General symptoms -
- Sharp pain at bite site
- Profuse sweating
- Nausea, vomiting and abdominal pain
Additional symptoms of a Funnel-Web bite -
- Copious secretion of saliva
- Muscular twitching - Breathing difficulty
- Breathing difficulty
- Small hairs stand on end
- Numbness around mouth
- Copious tears
- Disorientation
- Fast pulse
- Markedly increased blood pressure
- Confusion leading to unconsciousness
Additional symptoms of a RedBack Spider bite -
- Intense local pain which increases and spreads
- Small hairs stand on end
- Patchy sweating
- Headache
- Muscle weakness or spasms
Possible signs and symptoms of other spider bites/scorpion stings -
- Burning sensation
- Swelling
- Blistering
What to do:
First aid for Funnel-Web bite -
- Pressure bandage and immobilise
- Follow DRSABCD
- Call 000 for an ambulance
- Lie the patient down and ask them to keep still. Reassure the patient
- If bitten on a limb, apply an elasticised roller bandage (10–15 cm wide) over the bite site as soon as possible
- Apply a further elasticised roller bandage (10–15 cm wide), starting just above the fingers or toes and moving upwards on the bitten limb as far as can be reached
- Apply the bandage as firmly as possible to the limb. You should be unable to easily slide a finger between the bandage and the skin
- Immobilise the bandaged limb using splints
- Write down the time of the bite and when the bandage was applied. If possible, mark the location of the bite site (if known) on the skin with a pen, or photograph the site. Do not wash venom off the skin or clothes because it can assist identification
- Stay with the patient until medical aid arrives
First aid for RedBack Spider bite -
- Follow DRSABCD
- Lay the casualty down, rest and reassure
- Monitor the casualty constantly
- Apply a cold compress/cold pack to lessen the pain (no longer than 20 minutes)
Seek medical aid promptly, if:
- Person bitten is a young child, elderly, or infirmed
- The casualty collapses
- Pain is severe
First aid for all other spider bites/scorpion stings (Most dangerous are the Tarantula species, but also the Trapdoor species. There are no Mouse Spider species on the FNQ coast) -
- Wash the injured site with soap and water
- Apply a cold pack to the bitten or stung area for 15 minutes and reapply if pain continues
- Seek medical attention if the patient develops severe symptoms
Spinal Injury -
Spinal injury is damage to any part of the spinal cord. Injury to the spine interferes with the transmission of messages to and from the brain which may result in paralysis in the legs or arms. If the injury is very high up the spine, breathing can also be affected.
Caused by:
- Traffic-related accidents
- Workplace related accidents - Sporting accidents
- Sporting accidents
- Falls or hit by a falling object
- Significant blows to the head
Signs and symptoms:
- Pain at or below site of injury
- Tenderness or deformity
- Absent or altered sensation below site of injury e.g. tingling
- Loss of/or impaired movement below site of injury
- Nausea
- Headache or dizziness
- Breathing difficulties
- Altered conscious state
What to do:
Conscious casualty -
- Follow DRSABCD
- Rest and reassure
- Loosen tight clothing
- Support and hold head and neck in a neutral position, place hands on either side of the casualty’s head to prevent twisting or bending the spine
- Urgent medical aid. Call 000 for an ambulance
- If available, administer oxygen (this is known to extend the life of nerves at or near the injury)
Unconscious casualty -
- Follow DRSABCD
- If the casualty is breathing but remains unconscious, place them into the recovery position whilst holding the head and spine in a neutral position to prevent twisting or bending during movement
- Support head and neck in the neutral position place hands on either side of the casualty’s head to prevent twisting or bending the spine
- Maintain a clear and open airway
- Urgent medical aid. Call 000 for an ambulance
- If available, administer oxygen (this is known to extend the life of nerves at or near the injury)
Sprains and Strains -
A sprain is a severe wrench or twist of the ligaments, such as an ankle, wrist or another joint, that causes pain and swelling.
A strain is a force tending to pull or stretch muscles or tendons causing damage.
It can be difficult to tell whether the injury is a fracture, dislocation, sprain or strain. If in doubt, always treat it as a fracture.
Caused by:
- Falling and landing on arm
- Fall on the side of the foot
- Twisting a joint
Signs and symptoms:
- Pain
- Swelling
- Bruising
- Loss of power
- Tenderness
- Muscle spasm
What to do:
Conscious casualty -
- Rest and reassure the casualty
- Manage as a fracture if any doubt
- Follow the RICE management plan -
REST the casualty and the injured part
ICEPACK (cold compress) for 15 minutes
COMPRESSION bandage after the icepack - apply firmly and extend well beyond the injury
ELEVATE the limb
Rules when using icepacks -
- Wrap icepack in a damp cloth
- Apply to the injured site for 15 minutes and then reapply every 2 hours for first 24 hours
- Never apply ice directly to the skin or onto an open wound
- If no ice is available use a cloth wrung out in cold water - this will need replacing every 10 minutes
- Seek medical attention if in doubt or if no improvement after RICE
Unconscious casualty -
- Follow DRSABCD. Call 000 and request an ambulance
- Place patient in the recovery position, monitor breathing
- Follow RICE management plan if possible
Avoid HARM:
- Heat
- Alcohol
- Running or other exercise of the injured area
- Massage
Stinging Tree Sting -
Next to severe physical trauma, this is quite likely the most painful trial anyone can experience. There are two species present in the Greater Wangetti region -
Dendrocnide moroides - Stinging Bush (most commonly encountered)
Dendrocnide photinophylla - Shining-Leaved Stinging tree
Please see the "Dangerous Flora" page for details on the various species of Stinging Tree.
Stinging Mechanism:
All species of stinging trees have a similar stinging mechanism. The severity of the sting depends on the surface area of skin making contact with the leaf, the number of hairs on that leaf and the nature of the poison contained in the hairs. D. moroides - the venom is contained within tubular silica hairs which function as self-injecting hypodermic syringes after the tip breaks off on contact with the skin. On a large D. moroides leaf 30 cm by 20 cm there can be as many as 15,000 hairs on both sides of a single leaf (predominantly on the upper surface).
Note the little rounded tips on the hairs, which get knocked off on contact with the skin, and leave a beveled hypodermic needle-like end which easily punctures the skin. These spines are simply elaborate hairs - found on most plants
The Venom:
The composition of the venom is not understood but what is known is that it contains polypeptides which most likely stimulate the release of or mimic the actions of Acetylcholine, Histamines, 5-Hydroxtryptamine and Neuropeptides.
The exact nature of the toxins probably varies with different species. The stinging hairs of most nettle species contain formic acid, serotonin and histamine; however recent studies of Urtica thunbergiana (China) implicate oxalic acid and tartaric acid, at least in that species.
A polypeptide called moroidin has been isolated from D. moroides, and it is able to generate pain when minute doses are injected sub-dermally in human subjects - but it is still not as effective as the natural sting, indicating that a ‘cocktail of compounds are required', vis
-
Acetylcholine has a parasympathetic stimulant effect causing vasodilation of blood vessels in the skin and sweating
-
Histamine dilates the capillaries and increases capillary permeability leading to edema, erythema, and weals
-
5-Hydroxtryptamine (Serotonin) is a neurotransmitter involved in pain production and vasoconstriction
-
Neuropeptides, short chain proteins, probably cause the long term pain, hyperalgesia and sensitivity to temperature
-
Bradykinis, SRA, Leukotrienes and others
The surface of the silica hairs appear to be coated with a protein (which may be the polypeptide moroidin), which if the tubular hairs remain in the skin, causes long term hyperalgesia (an increased perception of pain and a lowered pain threshhold). This causes the untreated sting area to become very sensitive, especially in response to temperature changes, for many months after contact. These proteins (rather than the contents of the hairs) also appear to be largely responsible for the virulence of the pain
Effect of the Sting:
"If the leaves or the twigs make contact with the skin the hollow silica-tipped hairs penetrate and there is at first a slight itch, followed in a few seconds by a severe prickling effect which quickly becomes intense pain of a complex nature. The pain is described as composed of a background of tingling on which is superimposed an intermittant stabbing pain with sharp radiations passing in all directions. After a time, which varies in length, the stabs of sharper pain decrease in intensity and frequency but the diffuse background pain increases. The sharp tingling sensation is increased by touching, rubbing or cold. Referred pain in the thorax, chin, forehead, and in the opposite limb may also be experienced within 5 minutes of being stung. Pain also occurs frequently in the armpit or groin and this may persist for several days longer than the referred pain. The duller background pain may persist for several days and even after it finally disappears the affected portion may become extremely sensitive during cold weather or if rubbed or exposed to cold water. This effect may recur for 2 months or more after the original sting. Simultaneously with the production of pain the injured area quickly becomes covered with small red spots which join together and form a red swollen area surrounded by a flare zone. This effect appears within 5-10 minutes and persists for 8 hours or more. There is piloerection on the affected part generally intermittent and sometimes persisting for up to 30 hours. Sniffing and coughing have been reported in some cases."
Most effective treatment:
The acid and hairstrip technique -
Make up a solution of 3% hydrochloric acid in water
Hydrochloric acid (which is 30%) (commonly sold for cleaning cement and brickwork), produces very unpleasant choking fumes when concentrated, but is fine when diluted about 1 in 9 with water, which is what is used in this treatment. Hydrochloric acid is the acid produced by our stomachs (at about the same concentration that is used for the treatment).
The diluted acid will not harm the skin or most materials (but keep it away from metal utensils, use glass or plastic), however it stings quite intensely if it gets in cuts, so if you have cut or scratched hands, use a pair of latex throwaway gloves to apply it
Applying the acid
Use strips of tissue or toilet paper, laid over the affected area, and the acid poured over that to saturate the paper (and patted gently into close contact with the skin). It will sting intensely, for about 5 - 10 minutes, and then the sting will subside. Add a little more of the acid after about 10 minutes, and leave the tissues in place for at least 30 minutes
It must be emphasized that the victim should NEVER scratch the stung area - it breaks off the embedded stinging hairs and makes them difficult to remove later
For a light sting, this treatment is usually enough. For a bad sting, it will be necessary to use depilatory strips to remove the stinging hairs.
Application of wax
The aim of applying the wax is to remove as many of the stinging hairs as possible. With this end in mind the wax must be applied as gently as possible so as not to break off the brittle silica hairs making them almost impossible to remove. This is why Waxeeze is preferred over the conventional strips. In warm weather the wax can be spread with a knife like honey. In cold climates the Waxeeze may need to be warmed so it flows more easily.
Spread the wax directly on a linen strip, handkerchief, T-shirt, or whatever is available. Spreading the wax onto the cloth first minimizes the chances of breaking the hairs as would happen if you spread the wax directly onto the skin
Gently pat the linen on the affected area. The application of the wax can cause considerable pain in the short term but once the treatment is finished the pain quickly goes away
Leave the linen strip in place for five minutes to allow the body heat to soften the wax more and allow it to flow around the hairs providing better grip
After five minutes the cloth is ripped off in a fast movement. If possible rip the cloth off against the direction of the body hairs. This will remove the stinging hairs as well as the victim's own body hairs.
Repeat this procedure if the stinging hairs are not all gone. If all the new wax is used up linen strips can be reused
Immediately after the wax treatment Xylocaine or Lignocaine cream or similar can be applied to the affected area for pain relief
All pain can be expected to be gone by the next day although some itching has been reported. It is important that the victim does not scratch or rub. Antihistamines don't seem to reduce the severity of the pain but they might reduce the inflammatory responses.
Don't use the lotions sometimes included in the Waxeeze package as it contains chloroform which will make this type of pain worse
Nair, or other depilatory strips will work also
Hot water (as hot as is comfortably bearable) will also provide some relief
DO NOT USE -
Cunjevoi sap (ineffective)
Dettol (ineffective)
Urine (ineffective)
Cold water (will increase pain)
Alcohol (will increase pain)
While this technique works as a treatment, if there are symptoms such as asthma or other autonomic signs, consult a doctor
Stroke -
A stroke is a condition that occurs when an artery taking blood to the brain becomes blocked or bursts. As a result of a stroke, brain cells are damaged and functions controlled by that part of the brain are paralysed. Partial paralysis of the body and/or speech problems is common.
Recognise signs of a stroke:
FAST Stroke Assessment -
- Facial weakness
- Arm weakness
- Speech difficulty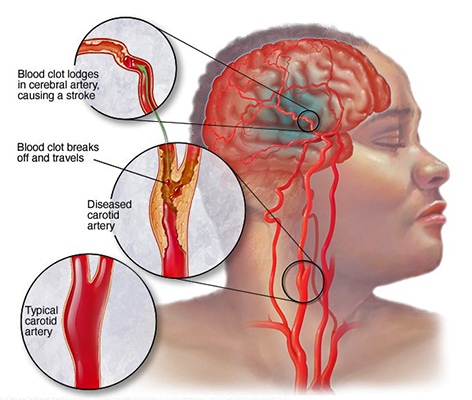
- Time to act fast!!
Caused by:
- Blocked arteries
- Blood clots
- Ruptured artery
Signs and symptoms:
- Sudden decrease in level of consciousness
- Weakness or paralysis on either one or both sides of the body
- Feeling of numbness in face, arm or leg
- Difficulty speaking or understanding
- Dizziness, loss of balance, unexplained fall
- Disturbed vision
- Confusion
What to do:
Conscious casualty -
- Follow DRSABCD
- Urgent medical aid. Call 000 for an ambulance
- Rest and reassure the casualty
- Place in a position of comfort and support the head and shoulders with pillows
- Loosen tight clothing
- Ensure airway is clear and open and wipe any secretions away from the mouth
- Do not give anything to eat or drink, as swallowing may be impaired
- Monitor casualty until medical aid arrives
Unconscious casualty -
- Follow DRSABCD
- Place into recovery position if unconscious and not breathing normally
- Urgent medical aid. Call 000 for an ambulance
Vertigo
Vertigo is a type of dizziness where you feel as though you or your surroundings are spinning, tilting or swaying.
Most dizziness is caused by problems of the inner ear which are treatable.
Sometimes dizziness can be caused by other conditions such as low blood pressure, some heart problems, anxiety or low blood sugar
Signs and symptoms:
- a sensation of movement (spinning, tilting, swaying) either of yourself or your surroundings
- unsteadiness, difficulty walking straight
- light-headedness
- feeling faint
Other symptoms can include:
- headache
- nausea and vomiting
- ringing sound in ears
- difficulty hearing
- staggering gait and loss of coordination
- jerky eye movements
- difficulty seeing clearly
What to do:
- Follow DRSABCD
- Help the casualty to sit or lie down in a comfortable position, and rest
- Advise the casualty to avoid abrupt head movements, especially looking up and making sudden changes in body position
- Provide the casualty with water to drink
- Turn off bright lights and ensure a flow of fresh air. Place patient in shade, if outdoors
- If this is the first time that the casualty has experienced dizziness or vertigo advise them to see their doctor
Keep the person safe:
- If standing or walking, help the casualty to avoid falling
- If the casualty feels nauseous or is vomiting, have them lie down on their side
- Do not allow the casualty to operate any machinery or drive